Overview
Our research is focused on optimising the diagnosis and management of patients with pubertal disorders.
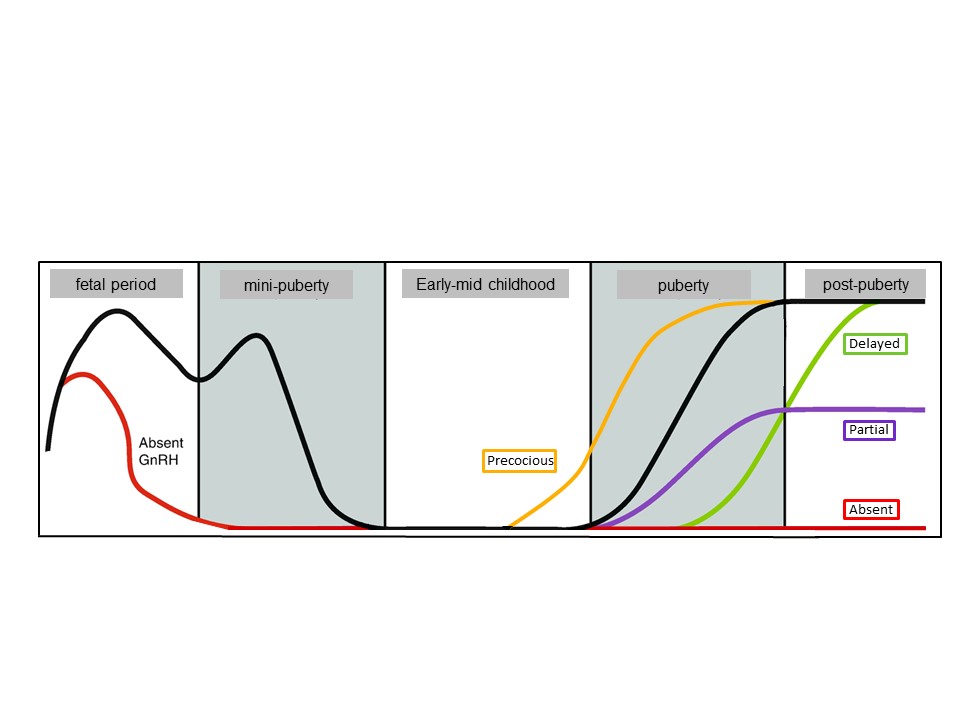
Puberty is the period of physical and psychological change from a child to an adult. Disorders of pubertal timing affect 4% of children, comprising significantly precocious (before 8-9yrs of age [>2 standard deviations below the mean population age]) or delayed (after 13-14yrs of age [>2 standard deviations above the mean age]) pubertal onset.
These common disorders are associated with adverse long-term health outcomes. Precocious puberty is associated with an increased risk of obesity, type 2 diabetes, and breast cancer, and delayed puberty is associated with psychosocial comorbidities and reduced bone density. Both are associated with early menopause or andropause.
While we know that these conditions often run in families, we still understand very little about how they occur and which gene changes are responsible. Currently, it can be difficult to distinguish which patients with early or late puberty need intensive treatment and follow up.
Genetics of Disordered Puberty Project:
- Central Precocious Puberty. Precocious puberty has historically been described as largely idiopathic, but recent evidence has described loss-of-function defects in neuroendocrine genes such as MKRN3 in familial precocious puberty. Through the latest genetic sequencing advances we aim to discover new genetic and biological causes of precocious puberty in order to help diagnose and understand the pathogenesis of this condition.
- Delayed Puberty. Conditions of delayed puberty exhibit a spectrum of severity, from 2-3 years delay in the timing of pubertal onset to an absolute failure of pubertal development. Whilst isolated delayed puberty affects 2% of the developed world, more severe disorders of the hypothalamic-pituitary-gonadal axis with gonadotropin deficiency are much rarer (1-10 per 10,000). Those patients with more significantly disordered puberty are more likely to have issues with fertility in adult life. We aim to identify gene defects that lead to late or absent puberty being passed down in families, in order to improve diagnosis and treatment of our patients.
Pubertal Induction with Gonadotropins in Male Adolescents with Absent or Arrested Puberty
In adolescents or young men who have not entered puberty due to a lack of GnRH or gonadotropin hormones (such as in Kallmann syndrome or idiopathic hypogonadotropic hypogonadism) puberty can be induced with either testosterone or gonadotropins (FSH and hCG). Gonadotropin therapy will lead to the development of secondary sexual characteristics in the same manner as testosterone, but also can faciliate future fertility potenital by allowing testicular cell development. Our group has developed a protocol for induction of puberty with gonadotropins for adolescent men with either no pubertal development or with initial pubertal development that has then arrested.
Mini-Puberty Induction with Gonadotropins (Mini-PInG) Study:
In patients with gonadotropin deficiency, poor response to adult fertility treatment is in part due to the absence of the infantile ‘mini-puberty’, during which reproductive hormone levels reach the adult range and reproductive capacity is established. We hypothesise that gonadotropin replacement in infancy in patients with severe GnRH deficiency results in improvement in reproductive capacity in adulthood.
We will carry out a study to understand the best hormones to use to treat babies with absent mini-puberty, to improve their potential for fertility as an adult.